How on-farm mastitis test helped farmer cut antibiotics use
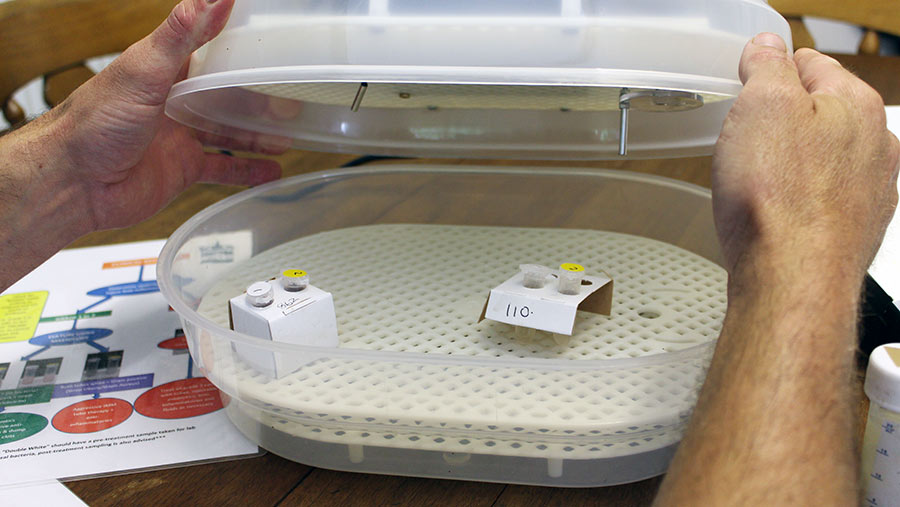
 A milk sample is put into two tubes containing a growth medium
A milk sample is put into two tubes containing a growth medium Rather than reaching for antibiotics at the first sign of mastitis, the team at Camerton Farm, Radstock, now do a milk bacteriology test for every case on farm and then make informed treatment decisions 14 hours later.
The approach is based on understanding the pathogens involved in causing a mastitis infection and then only using antibiotics to treat the bacteria that is likely to respond.
Infections that are likely to self cure will just receive non-steroidal anti-inflammatories (NSAIDs).
It is a strategy that was initially greeted with some scepticism by the team at Camerton, which is owned by the Wells family. However, a 45% reduction in repeat cases has laid any concerns to rest.
Camerton Farm facts
- 300 Holstein Friesians
- 9,500 litres a cow a year at 3.9% fat and 3.35% protein
- Arla Tesco contract
- Natural service
- Rear own replacements
- 854ha total, of which 172ha is grass used by the dairy and the rest in an arable rotation
See also: How a Shropshire dairy farmer saved £60,000 in mastitis control
Over the past 12 months, the policy has led to a 25% reduction in antibiotics tube use and a 34% drop in treated mastitis cases.
Mastitis improvements following milk bacteriology testing |
|||||
| 2017-2018 | 2018-2019 | Annual reduction | First six months of 2018-2019 | Second six months of 2018-2019 | |
| Antibiotics tube use for mastitis | 480 | 360 | -25% | 240 | 120 |
| Treated mastitis cases | 85 (32%) | 60 (21%) | -34% | 43 | 17 |
| Number of repeat cases | 20 | 11 | -45% | 10 | 1 |
|
In the first five months of 2018-19, samples were sent to the vets for analysis, which meant fewer samples were tested due to practicalities. In the past seven months, on-farm bacteriology testing was carried out, allowing more samples to be tested. This has resulted in bigger improvements (years run from June to June). |
|||||
Why the farm has taken this approach
Vet Charlie Neale of Shepton Vets says it’s about using antibiotics to the greatest affect.
“Quite a lot of research done recently has pointed towards mild to moderate cases of gram-negative bacteria being no more likely to cure with antibiotics therapy as self cure,” he explains.
This means it is likely that gram-negative infections – such as E coli – are generally being overtreated with antibiotics.
In comparison, Mr Neale explains that gram-positive bacteria, such as Strep uberis and Staph aureus, have been shown to respond better to aggressive antibiotics treatment, rather than short antibiotics courses.
This means these cases are possible being undertreated, potentially leading to more repeat infections.
Simon Wells says he was surprised at the small number of mastitis cases requiring antibiotics following bacteriology testing.
“Out of the first 20 tests we completed, 17 didn’t require antibiotics [gram-negative]. I realised we’d possibly been treating them for all this time for no reason and to no affect,” he says.

The-300-cow herd yields 9,500 litres a cow a year
How it works
Mr Wells started doing milk bacteriology tests about 12 months ago as part of an overall strategy to lower antibiotics use. He had already reduced use of critically important antibiotics and implemented selective dry cow therapy.
However, having identified mastitis as the main “weakness” for antibiotics use on farm, he was keen to look at strategies.

Simon Wells collects a clean milk sample from the cow and then uses a pipette to transfer milk into the agar test tubes
Initially, milk samples were packaged and sent back to Shepton Vets for testing. But the practicalities of sending samples meant not every case was sent for analysis and it could take about 24 hours to get a result.
Consequently, Mr Wells was keen to start doing on-farm testing. Mr Neale advised using the agar tube system MastDecide. This uses a set of two tubes containing a growth medium to determine what bacteria is present (see “Milk bacteriology testing using tube agars”).
Results are available within 14 hours, with treatment decisions then made.
On this farm, Mr Neale advised treating gram positive cases aggressively, potentially using off-label treatment to ensure an effective cure. Gram negative cases are monitored and given a NSAID.
The milk samples are incubated at 37C for 12-14 hours
Ultimately, the primary benefit of using on-farm kits is the ability to make faster, informed treatment decisions – something that is vital for treatment success.
Mr Wells believes on-farm testing has brought huge benefits. “It’s less milk thrown away, it helps the cow build up her own immunity and reduces antibiotics use by concentrating on tubing cows that will respond to it,” he says.
“I see it as similar to blanket treating dry cows with antibiotics in the past and now using selective dry cow therapy. It’s taken a while for everyone to do that. This will be similar.”
Milk bacteriology testing using tube agars
How to do it
- Put on a pair of clean disposable gloves.
- Pre-dip/spray teat and dry wipe.
- Discard first three strips of milk.
- Use cotton wool soaked in surgical spirit to clean teat end.
- Allow teat to dry and strip milk into sample tube – hold tube on a 45deg angle to minimise contamination.
- Ideally test immediately. If this is not possible, place in the fridge.
- Test the milk in a clean area.
- Wear a clean pair of gloves and use the exact volume pipette to take 0.1ml of milk. Squirt this into the first agar tube (white cap) and seal it. Repeat with the second tube (yellow cap).
- Label with cow ID.
- Place in the incubator at 37C for 12-14 hours (result may be seen as early as 8 hours).
Things to consider
- Before on-farm testing, carry out full bacteriology culturing through a vet to understand the main pathogens on farm.
- If you have more than 30 cases of mastitis per 100 cows, reduce this before doing on-farm testing.
- The agar tubes are not as accurate in determining specific pathogens as agar growth plates – which follow the same principles. However, the tubes are more farmer friendly, have a longer shelf life and provide a result within 12-14 hours, versus up to 48 hours with the plates.
- The tubes are slightly more expensive, although about the same price as vet analysis.
Interpreting milk bacteriology results |
||
|
Test medium 1 – white cap (general bacteria growth) |
Test medium 2 – yellow cap (gram-positive selective) | Test result |
| White | Pink | Gram-negative/coliforms (single pink) |
| White | White | White gram-postive (double white) |
| Pink | Pink | No bacteria growth (double pink) |
